Exploring the Cost and Frequency of Wellness Exams after ACA
April 12, 2016 •Heather Brotsos
 In this series of blog posts, we are using an all-payer claims database (APCD) from the state of New Hampshire to explore some questions related to the Affordable Care Act (ACA).
In this series of blog posts, we are using an all-payer claims database (APCD) from the state of New Hampshire to explore some questions related to the Affordable Care Act (ACA).
U.S. Department of Health and Human Services (HHS) provides a long list of all qualified preventive services. To start, we focus on one: the wellness exam. While there has been considerable debate around the merits of the annual physical, the wellness exam is the most common preventive service found in our claims data. So, we set out to investigate whether more people received wellness exams. Coverage without cost sharing for wellness exams went into effect September 23, 2010 for children and August 1, 2012 for women. Men do not qualify for coverage at no cost.
Which People Are getting wellness exams?
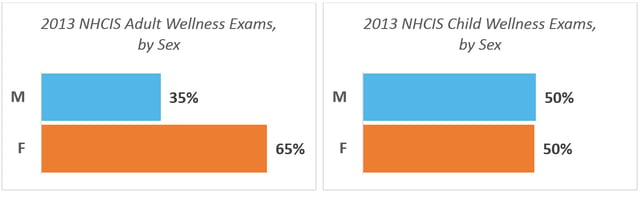
Twice as many women received a wellness exam as men in 2013. For children, utilization is split evenly between males and females.
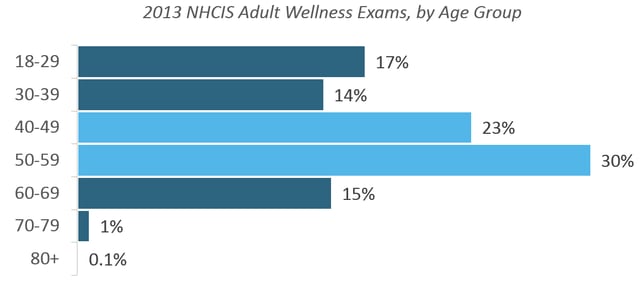
Over half of adult wellness exams in 2013 were provided to individuals between 40 and 59.
Which services are patients receiving at the wellness exam?
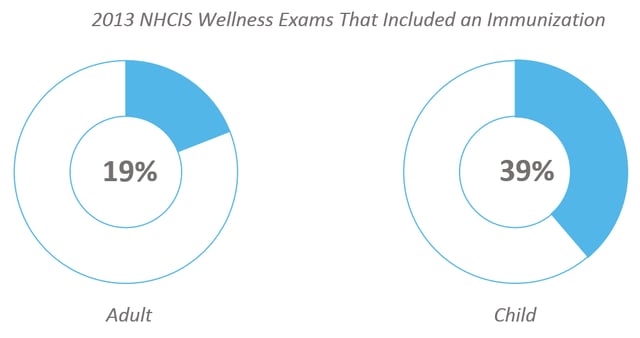
Patients received on average 1.15 additional services during the wellness visit in 2013 representing over 1,000 different procedure codes. Immunizations are the most common services provided during a wellness exam. In 2013, 39% of child and 19% of adult wellness exams included an immunization. Diagnostic tests (e.g. urinalysis, blood tests, and EKGs) cover the next most common procedures provided during a wellness visit.
Has patient cost sharing been reduced?
We examine average patient costs by year before and after the ACA went into effect[1]. In 2009, 27% of wellness exams were provided at no cost to the patient, compared to 80% in 2013.
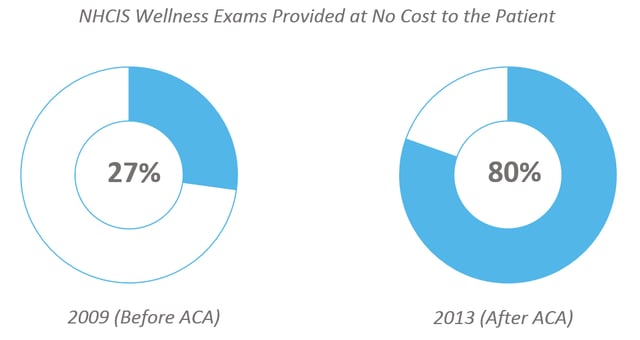
This trend is consistent across men, women and children. For all three groups, 27% of wellness exams are provided at no cost in 2009. In 2013, 83% of wellness exams for women are provided at no cost. This percentage is 77% for men and 76% for children in 2013.
Next, we looked at immunizations for evidence of a reduction in patient cost sharing. Since strong protocols already exist regarding many of these vaccines[2], we focus on three that are not compulsory for school enrollment or other reasons: shingles, human papillomavirus (HPV), and influenza. Coverage without cost sharing for all three of these vaccines went into effect September 23, 2010. Age and gender restrictions exist on both HPV and shingles vaccination. As mandated by the ACA, non-grandfathered plans must comply by offering these vaccines without patient cost sharing beginning in the next plan year.
We observe an increase in the percentage of vaccines provided at no cost to the patient for all three vaccines. The largest change is observed for the shingles vaccine. In 2009, 89% of vaccines were provided for free. In 2013, 99% were. The HPV vaccine sees an increase from 94% in 2009 to 99% in 2013. The Influenza vaccine has consistently had low patient cost sharing before and after ACA implementation. In 2009, 97% of these immunizations were provided at no cost to the patient, compared to 99% in 2013.
Through this initial analysis, we can conclude that there has been a reduction in patient costs for certain preventive services in New Hampshire between 2009 and 2013. It should be noted that while this coincides with the implementation of the ACA, we do not know whether the passage of the ACA caused the changes seen above. Also, the APCD only contains information for insured individuals and approved claims. As a result, our analysis does not include residents who receive benefits from the government, residents who have no insurance coverage, or claims that have been denied. Due to limitations in the data collection process, we are not able to assess changes in utilization over this time period.
Check back next week to learn about shifts in the insurance market after ACA.
Note: For all figures above, data for analysis includes public use data set acquired from New Hampshire Comprehensive Health Care Information System.
[1] Coverage for preventive services without cost sharing went into effect September 23, 2010 for most services. However, plans are not required to comply until the beginning of the next plan year. Exceptions exist for other circumstances, such as for grandfathered plans.
[2] For example, to attend public school, certain vaccines such as diphtheria, tetanus, and pertussis are required.
Get Updates
Featured Articles
Categories
- affordable housing (12)
- agile (3)
- AI (4)
- budget (3)
- change management (1)
- climate resilience (5)
- cloud computing (2)
- company announcements (15)
- consumer protection (3)
- COVID-19 (7)
- CredInsight (1)
- data analytics (82)
- data science (1)
- executive branch (4)
- fair lending (13)
- federal credit (36)
- federal finance (7)
- federal loans (7)
- federal register (2)
- financial institutions (1)
- Form 5500 (5)
- grants (1)
- healthcare (17)
- impact investing (12)
- infrastructure (13)
- LIBOR (4)
- litigation (8)
- machine learning (2)
- mechanical turk (3)
- mission-oriented finance (7)
- modeling (9)
- mortgage finance (10)
- office culture (26)
- opioid crisis (5)
- Opportunity Finance Network (4)
- opportunity zones (12)
- partnership (15)
- pay equity (5)
- predictive analytics (15)
- press coverage (3)
- program and business modernization (7)
- program evaluation (29)
- racial and social justice (8)
- real estate (2)
- risk management (10)
- rural communities (9)
- series - loan monitoring and AI (4)
- series - transforming federal lending (3)
- strength in numbers series (9)
- summer interns (7)
- taxes (7)
- thought leadership (4)
- white paper (15)